Researchers

Innovation

Precision

Science

Technology

Collaborations
Be a Part of Creating Neurosurgical Solutions
The goal of ClearPoint Neuro is to improve the patient’s quality of life by providing neuro interventional solutions with pinpoint accuracy. Our research is focused on cutting-edge innovation to address unmet pre-clinical and clinical needs across a wide spectrum of activities, including ideation, proof of concept, validation, and efficacy, while maintaining strong translational continuity across all services. We are committed to providing practical solutions to complex problems that can improve treatment specificity and effectiveness, patient outcomes, and clinical care.
Open Research Projects
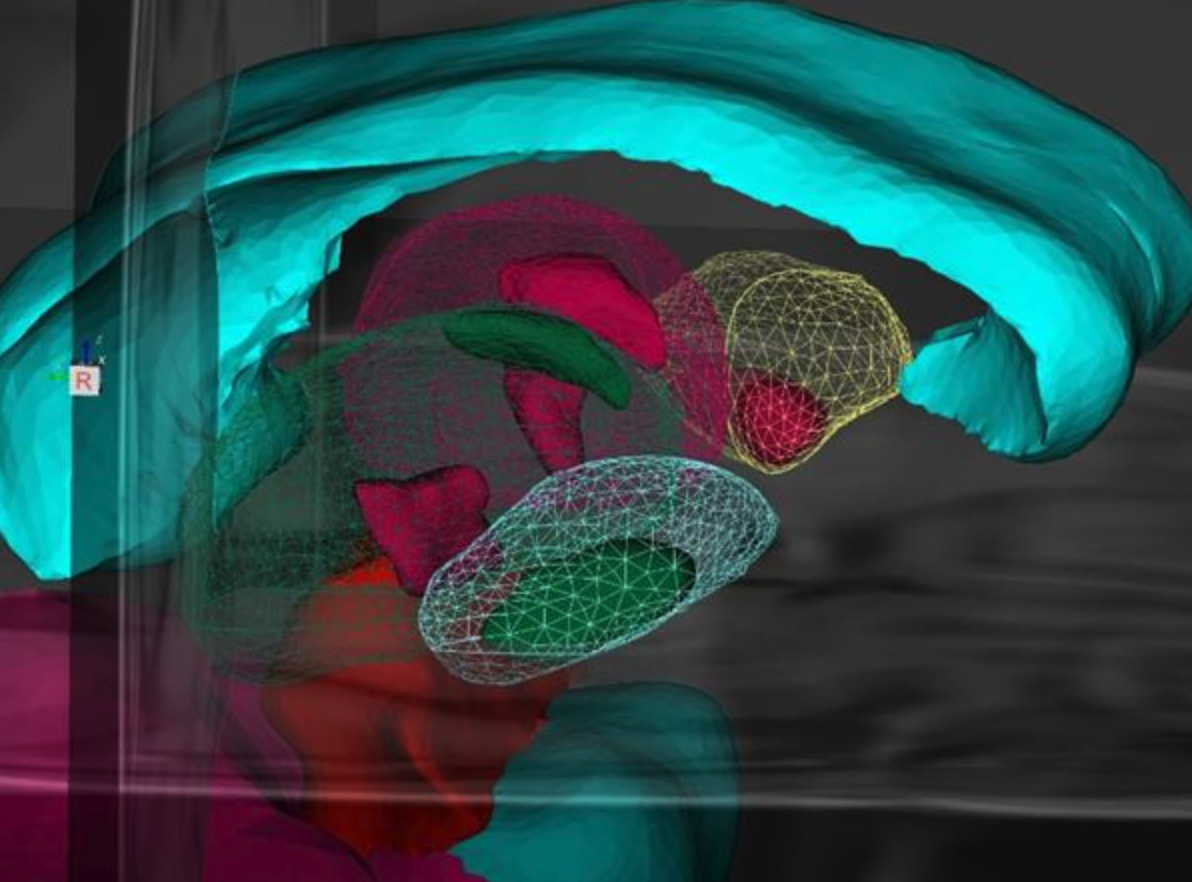
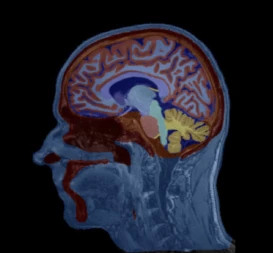
Model-Based Segmentation of Sub-Cortical Nuclei for Deep Brain Stimulation
L. Zagorchev PhD, N. Fläschner PhD, and F. Wenzel PhD
This work demonstrates not only that shape-constrained segmentation of sub-cortical nuclei from structural T1 MRI is feasible, but also that it can benefit minimally invasive surgical interventions. In addition to providing accurate and reproducible sub-cortical nuclei segmentation, the new method greatly enhances clinical workflows.
Featured partnerships & academic relationships
Open Projects in Development
Gene Therapy Infusion Coverage Tool Integration into ClearPoint Maestro® Brain Model
Worldwide agreement with NE Scientific, LLC.
ClearPoint Neuro is working with NE Scientific, LLC to develop a GPU-accelerated software solution into the ClearPoint Maestro® Brain Model for modeling of drug infusions delivered with the ClearPoint SmartFlow® cannula. This software collaboration will enable simulation of patient-specific infusion intra-procedurally to predict the distribution of therapeutic agents in 4D before the actual procedure to allow optimization of infusion parameters including target points, flow rate, infusion coverage and leakage outside of target-specific boundaries.
Fully Automatic Subnuclei Segmentation with ClearPoint Maestro® Brain Model for DBS
Worldwide license and research agreement with Philips.
ClearPoint Neuro is working with Philips to add subnuclei segmentation applied to MRI, and potentially CT scans, for use in the operating room. The design goal of the ClearPoint Maestro® Brain Model is to enable highly accurate ClearPoint interventions under both MRI and CT guidance by facilitating patient-specific, multi-modal fusion for accurate target identification and trajectory planning - Extending the software beyond the subcortical brain regions in Maestro to include segmentation of subnuclei from MRI to expand into the operating room.
Radially Branching Intra-Cerebral Cellular Delivery Device
Multi-year licensing agreement of intellectual property from UC San Francisco (UCSF) through its Innovation Ventures group.
ClearPoint Neuro is working with UCSF to develop and commercialize an innovative radially branching cellular delivery device for use both in the Operating Room under fluoroscopy/CT guidance as well as MRI-guidance. This device is being developed to help clinicians guide the delivery of biologic therapies — from stem cell transplants to gene therapy vectors — to specific locations in the human brain by helping surgeons tailor biologic delivery to individual patient anatomy and specific diseases.
Educational Resources for Researchers
The following resources are provided for educational and research purposes only. Please refer to our device labeling for more details on our approved label indications.
ClearPoint Peer-Reviewed Publications Bibliography
The ClearPoint Neuro Bibliography features ClearPoint in 70+ peer-reviewed publications.